Cook Children's Neurosciences Research Team Studies Brain Networks Connecting Epilepsy and Mental Health
People with epilepsy often suffer from comorbid mental health disorders, such as depression and anxiety. While this is thought to be a bidirectional relationship, research into how these conditions are connected and how they diverge is still ongoing, and in need of more vigorous research, merging behavior and brain function. Work led by Crystal Cooper, Ph.D., a principal investigator in the Neurosciences Research Center at the Jane and John Justin Institute for Mind Health at Cook Children's, aims to identify the neural correlates of cognitive processes thought to underlie psychiatric symptoms.
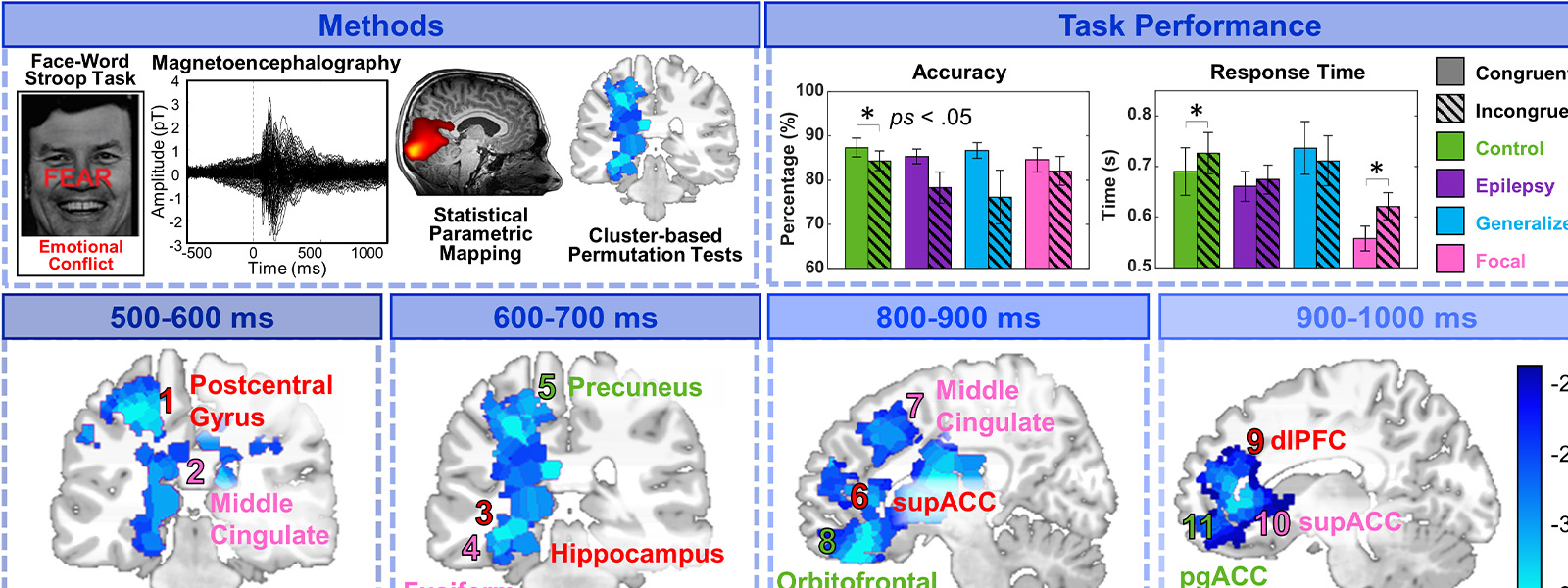
Published in Epilepsy and Behavior, Dr. Cooper's doctoral student, Kathryn King, was the first to identify the spatiotemporal profile of emotional conflict processing using magnetoencephalography (MEG). Emotion regulation is an important cognitive process that is impaired in individuals with psychiatric disorders. Less has been established in epilepsy, particularly in younger populations. The use of MEG allows mapping of where and when a given cognitive process occurs in the brain and, by studying different populations of children with and without epilepsy, we can understand how the differences in brain function may lead to different symptoms. Beyond the goal of identifying where and when brain function might be disrupted between those with and without epilepsy during emotional conflict processing – the goal was to also identify regions that predicted depression and anxiety symptoms in epilepsy, potentially leading to earlier recognition and treatment.
King et al., revealed that adolescents with epilepsy showed blunted brain responses to emotional conflict in regions related to error evaluation, learning and decision making. Furthermore, under activation in the error evaluation regions (e.g., cingulate) predicted anxiety and depression in focal epilepsy, while the regions related to learning (e.g., prefrontal cortex) predicted anxiety in generalized epilepsy. This may suggest differential mechanisms of dysfunction in these subgroups. Adolescents with epilepsy still exhibited deficits in emotional conflict processing in brain and behavioral responses despite similar rates of anxiety and depression across the groups. This may suggest that these deficits exist independently from psychopathology and may stem from underlying dysfunctions that predispose these individuals to develop both disorders. Findings such as these may provide potential targets for future research and therapies that isolate particular cognitive processes and brain networks.